Introduction to Leptospirosis
Leptospirosis is a bacterial infection that affects both humans and animals, caused by bacteria of the genus Leptospira. As a health specialist, it’s essential to understand this zoonotic disease, which can have serious health consequences if left untreated. Leptospirosis is a global public health concern, particularly in tropical and subtropical regions where the bacteria thrive in warm and wet environments. This comprehensive guide aims to provide an in-depth understanding of leptospirosis, its causes, symptoms, diagnosis, treatment, and prevention.
Causes of Leptospirosis
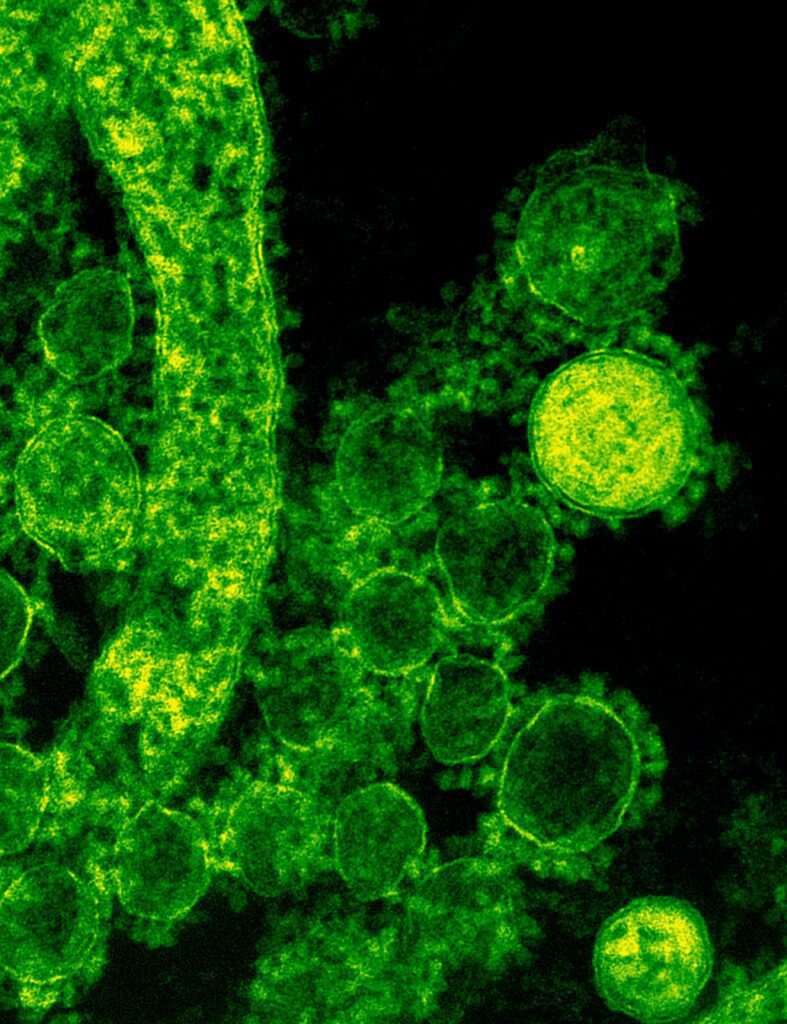
Bacteria responsible for Leptospirosis
Leptospirosis is caused by bacteria belonging to the Leptospira genus. Over 250 serovars (subtypes) have been identified, with each having different degrees of virulence and causing varying symptoms in both humans and animals. The most common serovars involved in human infections are Leptospira interrogans, Leptospira borgpetersenii, and Leptospira kirschneri. These spiral-shaped bacteria can penetrate the mucous membranes or broken skin and multiply rapidly, causing infection.
Transmission of Leptospirosis
The transmission of leptospirosis primarily occurs through direct or indirect contact with contaminated water, soil, or urine from infected animals. Common carriers of the bacteria include rodents, cattle, pigs, and dogs. High-risk environments include flooded areas, agricultural lands, and waste disposal sites. Occupations at higher risk of contracting the disease include farmers, veterinarians, sewage workers, and slaughterhouse workers. Ingestion of contaminated food or water, contact with open wounds or mucous membranes, and inhalation of aerosolized particles containing the bacteria can also lead to infection. Human-to-human transmission is extremely rare but has been reported in cases of vertical transmission from an infected mother to her fetus or through organ transplantation.
Symptoms and Stages of Leptospirosis
Early (acute) stage
After an incubation period of 2-30 days, the early stage of leptospirosis typically presents with flu-like symptoms, such as fever, chills, muscle aches, headache, and fatigue. Other possible symptoms include nausea, vomiting, diarrhea, abdominal pain, and a dry cough. This phase is known as anicteric leptospirosis and can last for about a week. It is important to recognize these symptoms as the initial signs of leptospirosis, as early diagnosis and treatment can prevent severe complications.
In some cases, patients may experience a temporary improvement in their condition before the disease progresses to a more severe stage. This biphasic pattern is commonly observed in leptospirosis infections.
Severe (icteric) stage
In a small percentage of cases, leptospirosis can progress to a more severe stage called Weil’s disease. This occurs when the bacteria invade multiple organs, including the liver, kidneys, lungs, and brain. Symptoms in this stage may include jaundice, kidney failure, respiratory distress, and hemorrhage. Weil’s disease carries a higher mortality rate and requires prompt medical attention and treatment.
In addition to Weil’s disease, severe cases of leptospirosis can also present with other complications, such as meningitis, uveitis, pulmonary hemorrhage, or rhabdomyolysis. These complications can lead to long-term health consequences, including chronic kidney disease, vision loss, and neurological disorders.
Diagnosis and Testing for Leptospirosis
Clinical diagnosis
Diagnosing leptospirosis can be challenging due to its non-specific symptoms and the possibility of co-infection with other diseases, such as dengue or malaria. A thorough patient history, including recent travel, occupational exposure, and contact with animals, can aid in clinical suspicion. Physical examination may reveal signs like conjunctival suffusion, muscle tenderness, and jaundice.
To improve diagnostic accuracy, healthcare professionals may use clinical scoring systems or predictive models, which take into account various factors such as patient demographics, symptoms, laboratory findings, and exposure history.
Laboratory testing
Laboratory testing is essential for confirming the diagnosis of leptospirosis. Blood, urine, and tissue samples may be collected and tested using various methods. Serological tests, such as the microscopic agglutination test (MAT), can detect the presence of antibodies against Leptospira. However, these tests may not be positive during the early stages of the disease, and cross-reactivity with other bacterial infections can sometimes lead to false-positive results.
Molecular tests, such as polymerase chain reaction (PCR), can detect the presence of the bacteria’s genetic material in the samples. These tests offer higher sensitivity and specificity compared to serological tests and can provide results within a few hours. However, the availability of PCR testing may be limited in resource-poor settings.
Other laboratory tests that may aid in the diagnosis of leptospirosis include blood cultures, enzyme-linked immunosorbent assay (ELISA), and immunofluorescence assays. Imaging studies, such as chest X-rays, ultrasound, or computed tomography (CT) scans, can help identify complications and assess the extent of organ damage.
Treatment and Management of Leptospirosis
Antibiotics
Antibiotics are the primary treatment for leptospirosis. Early administration of doxycycline or penicillin can effectively treat the infection and prevent severe complications. In cases of severe disease or allergy to first-line antibiotics, alternatives such as azithromycin or ceftriaxone may be used. It is crucial to start antibiotic therapy as soon as possible to reduce the risk of the disease progressing to a more severe stage.
Supportive care
Along with antibiotics, supportive care plays a vital role in the management of leptospirosis. Patients may require fluid replacement and electrolyte balance to address dehydration and maintain proper kidney function. In severe cases, oxygen therapy or ventilator support may be necessary to manage respiratory distress. Dialysis may be required for patients experiencing acute kidney failure.
Additional supportive care measures may include pain management, antipyretics to control fever, and antiemetics to manage nausea and vomiting. In cases of severe complications, such as pulmonary hemorrhage or meningitis, specific treatments like corticosteroids, intravenous immunoglobulin, or anticonvulsants may be considered.
Prevention and Control Measures
Personal protective measures
To reduce the risk of contracting leptospirosis, individuals working in high-risk environments or occupations should wear protective clothing and equipment, such as gloves, boots, and goggles. Proper hygiene and sanitation practices, including handwashing and avoiding contact with potentially contaminated water or soil, are essential. Additionally, handling animals with care and ensuring they receive proper veterinary care can help prevent the spread of the disease.
For those traveling to high-risk areas, taking doxycycline prophylactically may be recommended to reduce the risk of infection. However, this should be done under the guidance of a healthcare professional, as antibiotic prophylaxis is not appropriate for everyone.
Environmental control
Implementing rodent control measures, such as trapping and using rodenticides, can help minimize
the risk of leptospirosis transmission. Disinfecting contaminated areas with bleach or other disinfectants and safely disposing of animal waste can further reduce the chances of the bacteria spreading. Proper waste management, maintaining clean water sources, and reducing contact between humans and potential animal reservoirs are essential for controlling the spread of leptospirosis.
Community education and awareness programs can help promote responsible behavior and practices that minimize the risk of infection. Governments and local authorities must also implement public health policies and regulations to improve sanitation and control the disease in high-risk areas.
Vaccination and immunization
Vaccines for leptospirosis are available for animals, primarily livestock and pets, which can help reduce the spread of the disease. Regular vaccination of animals, particularly in high-risk areas, can contribute to overall disease control efforts.
While there is no human vaccine for leptospirosis, ongoing research aims to develop an effective and safe vaccine to protect individuals at high risk of exposure. Currently, experimental vaccines are being tested in clinical trials, and further advancements in vaccine development could significantly impact the global burden of leptospirosis.
Conclusion– Leptospirosis
Understanding leptospirosis and recognizing its symptoms and risk factors are essential for early diagnosis and treatment, which can ultimately save lives. Implementing personal protective measures, controlling environmental risks, and advocating for further research into human vaccination can significantly reduce the disease burden of leptospirosis. As a health specialist, it is our responsibility to educate and raise awareness about this potentially life-threatening disease and promote preventive measures to ensure the well-being of our communities.
By being vigilant and adopting appropriate prevention strategies, we can work together to reduce the impact of leptospirosis on global health. With ongoing research and collaboration between healthcare professionals, scientists, and public health officials, we can strive to develop new ways to combat this disease and protect the health and well-being of people worldwide.
Read more about:
How to treat Dandruff | Best Treatment of Rheumatoid Arthritis | Epiphyseal Plates | Excedrin Migraine | Treatments of Cervical Strain
Treatment of Chilblains | Benefits of Lemon Tea | Hair Transplant Cost | Benefits of Peanuts | Wrist Blood Pressure Monitor
Treatments of Morning Sickness | Benefits of Pomegranate Tea | Treatment of Asthma | Overhydration | Is whey protein safe to drink
Cerebral Infarction | Pomegranate Tea | How to survive Heart Attack | Benefits of Peanuts